Travelers are drawn to high altitude places in ever increasing number- Nepal alone now receives more than one hundred thousand trekkers from around the world every year. It can be easy to under-estimate the dangers of altitude illness; deaths from these conditions are all the more tragic because they are entirely preventable. Mountain climbers, serious trekkers, romantics sauntering through the foothills of the Himalayas, native porters, skiers in North America and Europe, pilgrims to high altitude shrines, diplomats posted to La Paz or Lhasa, miners in South America, and Everest marathon runners have something in common: they are all exposed to the effects of high altitude, and may be at risk from a potentially fatal but eminently preventable problem: Acute Mountain Sickness, commonly referred to just as AMS.
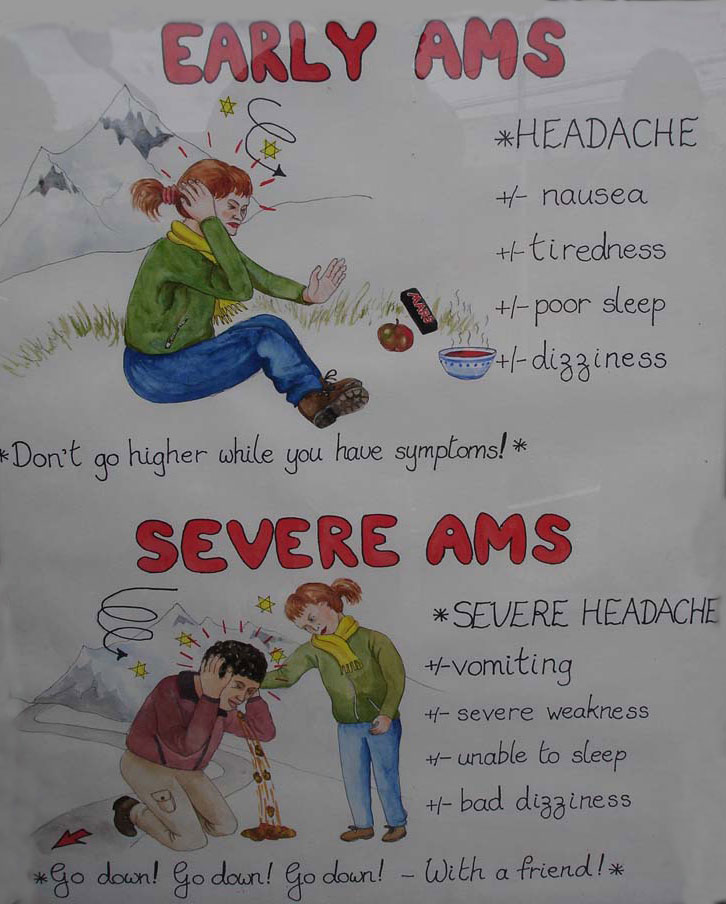
AMS consists of headache plus any one of the following symptoms in different degrees: nausea tiredness, sleeplessness or dizziness, occurring at altitudes of around 8000 ft or higher where pathophysiological changes due to lack of oxygen may manifest. Another term, “altitude illness’, is also widely used – an umbrella term that includes the benign acute mountain sickness and its two life-threatening complications, water accumulation in the brain (high altitude cerebral edema, HACE) or high altitude pulmonary edema (HAPE, water accumulation in the lungs). The latter two complications may follow AMS, especially when people continue to ascend in the face of increasing symptoms. In keeping with the Jesuit tradition of painstaking documentation, Father Joseph de Acosta, a sixteenth century Spanish Jesuit priest, is credited with having first described the effects of high altitude in humans. In vernacular Nepali, mountain sickness is called “lake lagne”: in Sanskrit it is aptly called “damgiri” (“dam” means breathlessness and “giri” means mountain).
Those most at danger from complications are people who do not “listen to their body”, and heed the early warning signals of AMS; they can go on to suffer from HAPE and HACE and may even die-a process that has been carefully documented in important autopsy studies performed by Walter Bond and John Dickinson during the Seventies in the old Shanta Bhawan hospital in Nepal.
Chronic mountain sickness is an entirely different condition, recognized by Carlos Monge Medrano in high altitude long-term residents of South America during the Twenties. Such maladaptation is seldom found in the Sherpas or Tibetans, possibly due to thousands of years of exposure to high altitude living. (south Americans populations are relative newcomers to high altitude.) The present discussion will be confined to acute exposure to altitude in short-term sojourners.
Mountain climbers, serious trekkers, romantics sauntering through the foothills of the Himalayas, native porters, skiers in North America and Europe, pilgrims to high altitude shrines, diplomats posted to La Paz or Lhasa, miners in South America, and Everest marathon runners have something in common: they are all exposed to the effects of high altitude, and may be at risk from a potentially fatal but eminently preventable problem: Acute Mountain Sickness, commonly referred to just as AMS.
If a participant on an Everest trek suffers from a mild headache and nausea at Namche Bazaar (12,300ft), he might take an asprin and wait for these symptoms to go away; however if the symptoms progress to vomiting and a splitting headache, he must assume that he is suffering from AMS and make plans to descend. It is amazing how many people in this situation ignore the dangers and continue to ascend with their friends, trying to blame their symptoms on poor fitness or flu. For some people, it’s the high investment of time, effort and money, for others perhaps it’s peer pressure or reluctance to accept defeat. A further is that many in the burgeoning adventure travel industry are clueless about mountain sickness.
AMS may set in within hours to days of arrival at high altitude: the onset of symptoms is usually gradual, which is why it is so vital to watch out for early warnings: does a person feel excessively tired; is she the last one to drag herself in to camp?
What causes AMS?
AMS is caused by a lack of oxygen. Although the proportion of oxygen in the atmosphere always remains the same (21%), as we go higher the “driving pressure” decreases. The driving pressure depends directly on the barometric pressure, and forces oxygen from the atmosphere into the capillaries of the lungs. Reduced driving pressure results in decreased saturation of oxygen in the blood and throughout the tissues.
Just what causes some people to suffer from AMS but not others is largely unknown, but there are clear-cut and important preventive factors that are now well- established (see below). The exact mechanism (pathophysiology) of AMS has similarities to that of HACE.
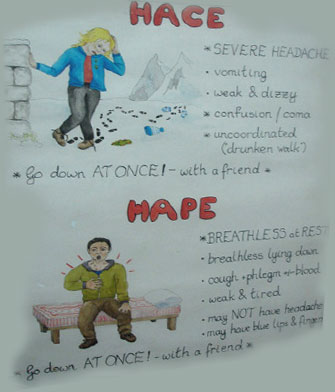
HIGH ALTITUDE CEREBRAL EDEMA (HACE)
Our trekker in the above example would probably go on to suffer form HACE if he continue to ascend despite the headache and vomiting; the symptoms of HACE are an extension of those to AMS.
From fatigue, there is progression to lethargy and then to coma. Or there may be confusion and disorientation, A useful test is to see if the person can walk a straight line. If he walks like a drunk or is unsteady, it has to be assumed that he has life-threatening HACE and needs to descend promptly with assistance. This situation is serious enough to justify immediate helicopter evacuation.
HACE is probably caused by shifts of fluid into the tissues of the brain. Reduced oxygen levels cause swelling within the confines of the bony skull. The resulting rise in pressure may lead to lethargy and eventually coma.
HIGH ALTITUDE PULMONARY EDEMA (HAPE)
This disease may follow AMS, but often it may appear independently. The typical scenario would be a trekker who has no headache or nausea, but finds he has a harder time walking uphill, that he is out of breath on slight exertion compared with the initial days of the trek. There may be a nagging cough and he too may have ascribed these symptoms to a cold. He may be suffering from sub-clinical or early HAPE, a well-recognized entity. With further ascent this may progress to shortness of breath even at rest – descend is now obligatory, or the outcome may be fatal.
Low oxygen causes the pulmonary artery to narrow and this results in exudation of blood near the smaller branches of the lungs (the alveoli). If the exudation continues, blood may escape into the alveoli leading to a cough with watery, blood-tinged phlegm. Such exudation, or “water logging” of the lung tissue interferes further with oxygenation. A popular, compact device called a pulse oximeter can measure the oxygen level in the blood simply and rapidly, using a sensor attached to the index finger. It can be very helpful in confirming if HAPE is present.
Acclimatization is a state of physiological “truce” between the body of a visitor and the hostile low-oxygen environment of high altitude. This truce permits the trekker of ascend gradually. (This is distinct from “adaptation” – permanent change to the organism, perhaps over thousands of years, perhaps even at a genetic or evolutionary level, to facilitate survival at altitude. Scientists are trying to decipher if the Sherpas or Tibetans have made such an adaptation.)
For acclimatization to take place the single most important step is hyperventilation- the trekker unconsciously breathes faster and more deeply than normal, even at rest, to make up for the lack of oxygen. However, hyperventilation also leads to loss of carbon dioxide from the blood, making the blood more alkaline, and it turn depressing ventilation. However, 48 to 72 hours after exposure to high altitude, the kidney comes to the rescue and begins to excrete alkali from the blood to restore a more balanced environment in which hyperventilation can continue unabated.
There is little doubt that altitude illness is one hundred percent a preventable illness. No one should die from it. For the past quarter of a century, one of the most important objectives of the Himalayan Rescue Association in Nepal has been to preach the gospel of prevention, from its aid posts in Pheriche (at around 14000ft in the Everest region) and Manang (at around 12000ft in the Annapurna region). There are four golden rules, plus some important general principles that should always be followed:
1. Understand and recognize the symptoms of AMS. Recent growth in adventure travel has made trekking at high altitude simpler and more accessible, with the result that more and more people who go trekking are ignorant of the basic facts of altitude illness.
2. Never ascend with obvious symptoms. Incredibly, I have known people who have hired a horse or a yak to go up higher when they were too sick to walk. This is courting disaster.
3. Descend if symptoms increase. It is amazing how striking and dramatic the relief may be with even a couple of hundred feet of descent. People with signs of HAPE or HACE have to descend.
4. Group members need to look out for one another (perhaps like the buddy system in SCUBA diving). This rule gets broken with unfailing regularity every trekking season in the Himalayas, because people are just too anxious to complete their trek, even if one of their party members is ill. A trekker with AMS, HAPE Or HACE will want nothing more than to be left alone, unbothered, at the same Altitude- potentially a fatal option. There is no alternative but to bring the person down to a lower altitude accompanied by a friend who speaks the same language.
Following a conservative rate of ascent
Going too high, too quickly, is the single most important cause of susceptibility to AMS. Beyond about 9000ft, the sleeping altitude should be no higher than about 1500ft from the previous night’s altitude. The sleeping altitude, not the altitude achieved during the daytime, is what is important. Altitude sickness often manifests at night because during sleep the oxygen level in the blood may dip further. Many mountain climbers will have been to 14000ft or high in the Alps or in North America but few will have slept at the altitude. In the Himalayas, you don’t have to be an experienced climber, or use crampons, to be able to “hang out” at 15000ft or higher for days: easy accessibility to these altitudes makes exposure to AMS also mush easier.
While ascending, every second or third day should be rest day for acclimatization. “Climb high and sleep low” is the dictum, but it is important not to exert oneself excessively in trying to fulfil this.
The trekker should not be in a hurry in the mountains. The itinerary should be planned so that there are enough “leeway days” in case more time is needed to acclimatize. Trying to do a high-altitude two-week trek in one week is always fraught with problems.
Avoiding of excessive exertion in the initial days
Excessive physical exertion at high altitude makes one more susceptible to AMS. It is important to take it easy at high altitude, especially in the initial days. People who are very fit for example marathon runners or those who carry very heavy backpacks seem more vulnerable to AMS than others, probably because they push themselves harder. I once looked after a trekker who felt he could not break his morning jogging sessions despite a strenuous trek day ahead, even at 4000m! The feeling of” man against nature” may be stronger in this fitter group.
Avoiding alcohol
Jim, a rock star, decided to “whoop it up” with four bottles of beer, on arrival at 3500meters in the Everest region. He felt ill with severe AMS and needed to be helicoptered out two days later. He had been warned not to drink alcohol on the trek, especially while ascending. Alcohol may dehydrate the trekker but more importantly it depresses breathing or ventilation. Sleeping pills may have a similar effect.
Maintaining adequate hydration
Adequate amounts of fluid (about 3 liters a day) are necessary in the mountains:- dehydration mimics altitude sickness and may even predispose to it. On the other hand excessive water drinking should also be avoided as this may lead to electrolyte imbalances.
Maintaining a high carbohydrate diet
A high carbohydrate diet aids ventilation and efficient use of oxygen. The good news is that – in many high altitude places – there is not much alternative: rice, potatoes and other strach-laden foodstuffs tend to be the staple, with not much else to choose from.
Drug prevention (prophylaxis)
Diamox (actazolamide) may be necessary for people going on rescue missions at high altitude or flying in to high altitude cities like La Paz or Lhasa. People with sulpha allergy should not take diamox, the primary drug for prevention, and further details are given below. A second drug, dexamethasone (see below) should also be carried, particularly if the destination is remote: this can be life saving if HACE supervenes.
Descent
Wherever, possible this has to be attempted. There is really no magic altitude to descend, but the sick patient may suddenly feel something lift and feel hungry. This is the altitude to which the body is adjusted. Patients with HAPE need to descend slowly and with assistance: excessive exertion even during descent may increase the blood flow to the lungs and exacerbate the problem.
Oxygen
Lack of oxygen at altitude is the chief reason why people suffer from altitude sickness, so breathing supplemental oxygen is obviously going to make a difference. But oxygen is a hard commodity to come by in the mountain – cylinders of oxygen are not easily portable. When oxygen available in AMS settings, it should be used.
Drugs
Acetazolamide (diamox): This is the most tried and tested drug for altitude sickness prevention and treatment. Unlike dexamethasone this drug does not mask the symptoms but actually treats the problem. It seems to works by increasing the amount of alkali (bicarbonate) excreted in the urine, making the blood more acidic. Acidifying the blood drives the ventilation, which is the cornerstone of acclimatization.
For prevention, 125 mg twice daily starting the evening before and continuing for three days once the highest altitude is reached, is effective. A recent article in the British Medical Journal suggested taking a higher dosage — 750mg daily. Our experience in the Indian subcontinent has consistently been that 250 mg per day has been rewarding, while excessive dosage may just increase the side effects.
Side effects of diamox are: an uncomfortable tingling of the fingers, toes and face (called “jhum jhum” in Nepali); carbonated drinks tasting flat; excessive urination; and rarely, blurring of vision. In most of the treks in Nepal, gradual ascent is possible and prophylaxis tends to be discouraged. Certainly if trekkers develop headache and nausea or the other symptoms of AMS, then treatment with diamox is fine. The treatment dosage is 250 mg twice a day for about three days.
Dexamethasone: This steroid drug can be life saving in people with HACE, and works by decreasing swelling and reducing the pressure in the bony skull. The dosage is 4 mg three times per day, and obvious improvement usually occurs within about six hours. Like the hyperbaric bag (See below), this drug “buys time” especially at night when it may be problematic to descend. Descent should be carried out the next day. It is unwise to ascend while taking dexamethasone: unlike diamox this drug only masks the symptoms
Dexamethasone can be highly effective: many people who are lethargic or even in coma will improve significantly after tablets or an injection, and may even be able to descend with assistance. Many pilgrims at the annual festival at Gosainkunda lake in Nepal suffer from HACE following a rapid rate of ascent, and respond remarkably well to dexamethasone. Mountain climbers also sometimes carry this drug to prevent or treat AMS. It needs to be used cautiously, however, because it can cause stomach irritation, euphoria or depression.
It may be a good idea to pack this drug for a high altitude trek for emergency usage in the event of HACE In people allergic to sulpha drugs (and therefore unable to take diamox) dexamethasone can also be used for prevention: 4 mg twice a day for about three days may be sufficient.
Nifedipine: This drug is generally used to treat high blood pressure, but also seems able to decrease the narrowing in the pulmonary artery caused by low oxygen levels, thereby improving oxygen transfer. It can therefore be used to treat HAPE, though unfortunately its effectiveness is not anywhere as dramatic that of dexamethasone in HACE. The dosage is 20 mg of long acting nifedipine, six hourly.
It can cause sudden lowering of blood pressure so the patient has to be warned to get up slowly from a sitting or reclining position. It has also been used in the same dosage to prevent HAPE in people with a past history of this disease.
The hyperbaric bag
This is a simple, effective device, made of airtight nylon; it is about 7 feet long ad looks like a long duffel bag. With the patient inside, the bag is inflated with a foot pump until it becomes like a large sausage-shaped balloon. There is a one-way valve to avoid carbon dioxide build up inside, and it has transparent panels to assist communication with its occupant.
The pressure inside the bag is 2 p.s.i,. so the effect is about the same as bringing the patient down a couple of thousand feet. For both HACE and HAPE (but especially, in our experience, for HACE) the changes are usually dramatic within an hour. However there may be a “rebound” tow or three hours after therapy and the patient may need to get in the bag again. Just like the dexamethasone, this bag only helps to “buy time”. Descent is still mandatory as soon as possible.
Periodic breathing
An abnormal breathing pattern whilst asleep is a common occurrence at high altitude: short spells of an increased breathing rate alternate with brief periods when breathing slows down seems to stop the medical term for this is “Cheyne Stokes” respiration. It is only a problem if it makes the suffers wake up repeatedly, breathless, anxious and unable to sleep. An effective remedy is Diamox 125 mg before dinner, which counteracts the low oxygen dips during sleep that trigger the problem. Sleeping pills should be avoided.
Upper respiratory tract infections and symptoms
Many people develop a persistent, bothersome cough and cold-like symptoms in the cold dry air of high altitude. An antihistamine at night like Benadryl 25 mg may help suppress the cough. Antibiotics are sometimes useful, but keeping the head and face covered and breathing through a silk or wool scarf to humidify the air may also help. many studies have shown that upper respiratory tract infections can predispose to AMS.
Peripheral edema
There may be swelling around the eyes, fingers, ankles at high altitude, but this may not indicate AMS per se unless accompanied by the symptoms of AMS. These symptoms without AMS usually require no treatment.
High altitude syncope (fainting): This is well known but harmless problem, in which fainting occurs suddenly, usually shortly after arrival. Simple measures like keeping the individual in a reclining position and raising the legs is helpful.
Travelers with pre-existing health problems; children, and birth control pills
High blood pressure: Blood pressure initially increases at high altitude due to the initial stress of low oxygen triggering neurohumoral changes. However people who suffer from high blood pressure can go up to high altitude as long as this is well controlled and they continue to take their medication.
Coronary heart disease: People with a history of heart attack (moycardial infarction) and even those with coronary artery bypass grafts or angioplasty but with no angina, can trek up to high altitude provided they are fit and able to walk rigorously at low altitude. The high altitude does not seem to add any extra burden to the heart.
Epilepsy: Although seizures may be provoked by altitude there is no convincing evidence that it is unsafe for well-controlled epileptics travelling to travel to high altitude, though such people should always take their anti seizure medications conscientiously.
Migraine: Sufferers may possibly have more attacks in the mountains and this may sometimes be difficult to distinguish from AMS. In doubt it is best to descend.
Lung disease: Also noteworthy is the limited observation that bronchial asthma does not seem to get exacerbated at high altitude due to the cold and exercise. However it is prudent for asthmatics to carry inhalers and other medications. Obviously people with chronic obstructive lung disease may be more short of breath and travel at high altitude would be inadvisable.
Neck surgery and radiotherapy: People with treated cancers like lymphoma or tumors in the neck who have had extensive surgery or radiation treatment may be especially prone to AMS because of damage to the carotid bodies – tiny organs within the carotid arteries that sense oxygen and aid ventilation.
Diabetes: Diabetics on insulin should have a reliable glucometer to check their blood glucose regularly, but high altitude does not seem to cause additional risks.
Corneal surgery: people who have had non laser surgery (radial keratotomy) to correct their short sightedness may run into problems at high altitude due to swelling of their cornea caused by the low oxygen. Such people should carry corrective lenses as well if travelling to high altitude.
Pregnancy: Pregnant women should not sleep higher than 12000ft as this may endanger the fetus; a further problem is that high altitude places are generally remote, making emergencies more difficult to deal with.
Children: Children do not suffer any more from the effect of altitude than adults. However, it is important that a child should be able to communicate any symptoms to responsible adult, so that prompt descent can be arranged. It may therefore be dangerous to take children to high altitude that is not yet old enough to do this.
Contraception: Oral contraceptive pills may predispose to abnormal blood clotting (thrombosis) at high altitude. the hypoxia (low oxygen), the excessive red blood cells (polycythemia) in the blood, and the possible dehydration in this environment may already be other predisposing factors for thrombosis. Hence it if best to use other forms of contraception at high altitude.
Other disease risks
Many high altitude destinations are in developing countries, so it is important to be up to date with vaccinations against disease like typhoid and hepatitis, to know about travelers’ diarrhoea and its treatment, and to understand the other precautions described elsewhere in this book. Malaria is not a risk at altitude – transmission does not take place above 2000 meters.
Conditions that mimic altitude sickness
Improving medical facilities in countries such as Nepal have made it much easier to distinguish between altitude illness and conditions that can produce similar symptoms, such as bleeding in the brain (subarachnoid hemorrhage), strokes, dehydration and blood viscosity related problems like venous thrombosis.
Porters in the Himalayas
It is important to be aware that porter may be just as vulnerable to the effects of altitude as tourist; for your own safety, it is also vital to confirm with the trekking agency that your porter has been provided with proper clothing, boots and equipment prior to the start of the trek.
Conclusion
Most of the problems of high altitude are totally preventable. With careful precautions, your experience in the mountains should be safe and rewarding.